Welcome to our endometriosis website, where we'll explore this condition in a way that's easy to understand and relatable to you. Imagine having a friend who's been through the challenges of endometriosis and is here to guide you.
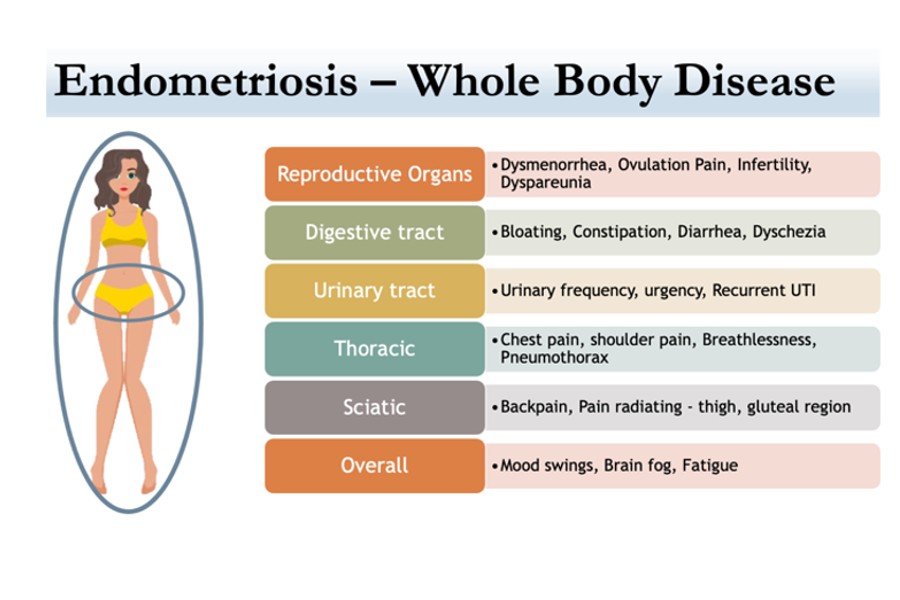
Endometriosis, in simple terms, is a common and incredibly painful condition that affects about 1 in 10 women. It can strike anyone from their teenage years to menopause, causing a range of symptoms that impact various parts of the body. While it used to be seen primarily as a reproductive issue, we now understand that it's a whole-body condition, bringing with it a host of associated symptoms.
Think of endometriosis as a mystery waiting to be unraveled. On this website, we aim to provide answers to the questions you may have about endometriosis, making this journey a bit less daunting for you. So, let's explore together and find the support and knowledge you need.